|
Dr. Nath Publications.
Selected List

|
Improvement in abduction of the shoulder after reconstructive soft-tissue procedures in obstetric brachial plexus palsy.
Authors :Nath RK, Paizi M.
|
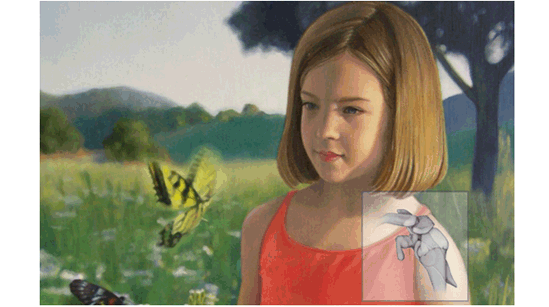
Residual muscle weakness in obstetric brachial plexus palsy results in soft-tissue contractures which limit the functional range of movement and lead to progressive glenoid dysplasia and joint instability. We describe the results of surgical treatment in 98 patients (mean age 2.5 years, 0.5 to 9.0) for the correction of active abduction of the shoulder. The patients underwent transfer of the latissimus dorsi and teres major muscles, release of contractures of subscapularis pectoralis major and minor, and axillary nerve decompression and neurolysis (the modified Quad procedure). The transferred muscles were sutured to the teres minor muscle, not to a point of bony insertion. The mean pre-operative active abduction was 45 degrees (20 degrees to 90 degrees ). At a mean follow-up of 4.8 years (2.0 to 8.7), the mean active abduction was 162 degrees (100 degrees to 180 degrees ) while 77 (78.6%) of the patients had active abduction of 160 degrees or more. No decline in abduction was noted among the 29 patients (29.6%) followed up for six years or more. This procedure involving release of the contracted internal rotators of the shoulder combined with decompression and neurolysis of the axillary nerve greatly improves active abduction in young patients with muscle imbalance secondary to obstetric brachial plexus palsy.

|
Upright MRI of glenohumeral dysplasia following obstetric brachial plexus injury.
Authors :Nath RK, Paizi M, Melcher SE, Farina KL.
|
The purpose of this study was to evaluate the role of upright magnetic resonance imaging (MRI) shoulder scanning in the diagnosis of glenohumeral deformity following obstetric brachial plexus injury (OBPI). Eighty-nine children (ages 0.4 to 17.9 years) with OBPI who have medial rotation contracture and reduced passive and active lateral rotation of the shoulder were evaluated via upright MRI of the affected glenohumeral joint. Qualitative impressions of glenoid form were recorded, and quantitative measurements were made of glenoid version and posterior subluxation. Glenoid version of the affected shoulder averaged -16.8+/-11.0 degrees (range, -55 degrees to 1 degrees ), and percentage of the humeral head anterior to the glenoid fossa (PHHA) averaged 32.6+/-16.5% (range, -17.8% to 52.4%). The glenoid form was normal in 43 children, convex in 19 children and biconcave in 27 children. Standard MRI protocols were used to obtain bilateral images from 14 of these patients. Among the patients with bilateral MR images, glenoid version and PHHA were significantly different between the involved and uninvolved shoulders (P<.000). Glenoid version in the involved shoulder averaged -19.0+/-13.1 degrees (range, -52 degrees to -3 degrees ), and PHHA averaged 29.7+/-18.4% (range, -16.2% to 48.7%). In the uninvolved shoulder, the average glenoid version and PHHA were -5.2+/-3.7 degrees (range, -12 degrees to -1 degrees ) and 47.7+/-3.0% (range, 43% to 54%), respectively. The relative beneficial aspects of upright MRI include lack of need for sedation, low claustrophobic potential and, most important, natural, gravity-influenced position, enabling the surgeon to visualize the true preoperative picture of the shoulder. It is an effective tool for demonstrating glenohumeral abnormalities resulting from brachial plexus injury worthy of surgical exploration.

|
Surgical correction of unsuccessful derotational humeral osteotomy in obstetric brachial plexus palsy: evidence of the significance of scapular deformity in the pathophysiology of the medial rotation contracture.
** Free **
Authors :Nath RK, Melcher SE, Paizi M.
|
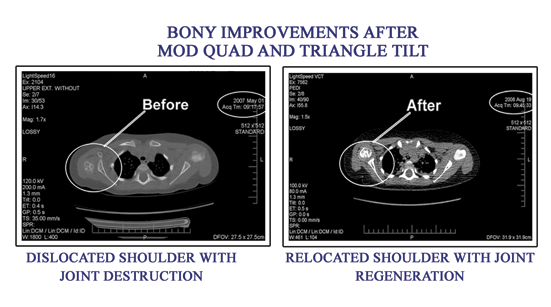
BACKGROUND: The current method of treatment for persistent internal rotation due to the medial rotation contracture in patients with obstetric brachial plexus injury is humeral derotational osteotomy. While this procedure places the arm in a more functional position, it does not attend to the abnormal glenohumeral joint. Poor positioning of the humeral head secondary to elevation and rotation of the scapula and elongated acromion impingement causes functional limitations which are not addressed by derotation of the humerus. Progressive dislocation, caused by the abnormal positioning and shape of the scapula and clavicle, needs to be treated more directly. METHODS: Four patients with Scapular Hypoplasia, Elevation And Rotation (SHEAR) deformity who had undergone unsuccessful humeral osteotomies to treat internal rotation underwent acromion and clavicular osteotomy, ostectomy of the superomedial border of the scapula and posterior capsulorrhaphy in order to relieve the torsion developed in the acromio-clavicular triangle by persistent asymmetric muscle action and medial rotation contracture. RESULTS: Clinical examination shows significant improvement in the functional movement possible for these four children as assessed by the modified Mallet scoring, definitely improving on what was achieved by humeral osteotomy. CONCLUSION: These results reveal the importance of recognizing the presence of scapular hypoplasia, elevation and rotation deformity before deciding on a treatment plan. The Triangle Tilt procedure aims to relieve the forces acting on the shoulder joint and improve the situation of the humeral head in the glenoid. Improvement in glenohumeral positioning should allow for better functional movements of the shoulder, which was seen in all four patients. These dramatic improvements were only possible once the glenohumeral deformity was directly addressed surgically.

|
Scapular deformity in obstetric brachial plexus palsy: a new finding. ** Free **
Authors :Nath RK, Paizi M.
|
While most obstetric brachial plexus palsy patients recover arm and hand function, the residual nerve weakness leads to muscle imbalances about the shoulder which may cause bony deformities. In this paper we describe abnormalities in the developing scapula and the glenohumeral joint. We introduce a classification for the deformity which we term Scapular Hypoplasia, Elevation and Rotation. Multiple anatomic parameters were measured in bilateral CT images and three-dimensional CT reconstruction of the shoulder girdle of 30 obstetric brachial plexus palsy patients (age range 10 months-10.6 years). The affected scapulae were found to be hypoplastic by an average of 14% while the ratio of the height to the width of the body of scapula (excluding acromion) were not significantly changed, the acromion was significantly elongated by an average of 19%. These parameters as well as subluxation of the humeral head (average 14%) and downward rotation in the scapular plane were found to correlate with the area of scapula visible over the clavicle. This finding provides a classification tool for diagnosis and objective evaluation of the bony deformity and its severity in obstetric brachial plexus palsy patients.

|
Physiological and clinical advantages of median nerve fascicle transfer to the musculocutaneous nerve following brachial plexus root avulsion injury.
Authors : Nath RK, Lyons AB, Bietz G.
|
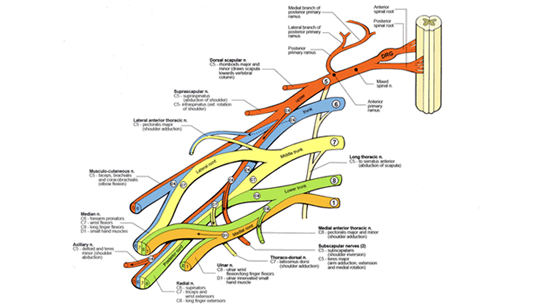
OBJECT: Loss of biceps muscle function is a significant disability after brachial plexus root avulsion injuries. Nerve grafting techniques to reestablish anatomical and functional continuity between the spinal cord and the avulsed root have not proven successful. Using nerve transfers for functional restoration of root avulsion injuries appears to be effective and has physiological advantages for reducing regeneration distances. Since the early 1990s, the Oberlin technique of transferring ulnar nerve fascicles to the motor branch of the musculocutaneous nerve has been the preferred operative technique for reinnervation and restoration of biceps muscle function. In the current study the authors examine the efficacy of an alternative technique using median nerve fascicles transferred to the musculocutaneous nerve to reinnervate the biceps muscle. METHODS: Forty consecutive patients with combined C5-6 brachial plexus root avulsions were evaluated pre- and postoperatively according to the British Medical Research Council Motor Grading Scale. Personal interviews concerning quality of life (QOL) after surgery were conducted and scored based on standards set by the World Health Organization. All patients showed some degree of improvement in biceps muscle function. Thirty-six (90%) of the 40 patients regained movement against gravity. The patients had a 77% improvement in overall QOL after the surgery; most notably, 92% of the patients reported their lack of need for medication and 75% a significant lessening of postoperative pain. Redirection of part of the healthy median nerve resulted in no measurable functional deficits, and only 28 patients reported minor sensory disturbances in the first web space for an average of 3 months after surgery. CONCLUSIONS: Median nerve fascicle transfer resulted in a significant improvement in biceps muscle function with an acceptable level of morbidity and should be considered an effective, and in many cases preferable, alternative to ulnar nerve fascicle transfer.

|
Microneurolysis and decompression of long thoracic nerve injury are effective in reversing scapular winging: long-term results in 50 cases. ** Free **
Authors: Nath RK, Lyons AB, Bietz G.
|
BACKGROUND: Long thoracic nerve injury leading to scapular winging is common, often caused by closed trauma through compression, stretching, traction, direct extrinsic force, penetrating injury, or neuritides such as Parsonage-Turner syndrome. We undertook the largest series of long thoracic nerve decompression and neurolysis yet reported to demonstrate the usefulness of long thoracic nerve decompression. METHODS: Winging was bilateral in 3 of the 47 patients (26 male, 21 female), yielding a total of 50 procedures. The mean age of the patients was 33.4 years, ranging from 24-57. Causation included heavy weight-lifting (31 patients), repetitive throwing (5 patients), deep massage (2 patients), repetitive overhead movement (1 patient), direct trauma (1 patient), motor bike accident (1 patient), and idiopathic causes (9 patients). Decompression and microneurolysis of the long thoracic nerve were performed in the supraclavicular space. Follow-up (average of 25.7 months) consisted of physical examination and phone conversations. The degree of winging was measured by the operating surgeon (RKN). Patients also answered questions covering 11 quality-of-life facets spanning four domains of the World Health Organization Quality of Life questionnaire. RESULTS: Thoracic nerve decompression and neurolysis improved scapular winging in 49 (98%) of the 50 cases, producing "good" or "excellent" results in 46 cases (92%). At least some improvement occurred in 98% of cases that were less than 10 years old. Pain reduction through surgery was good or excellent in 43 (86%) cases. Shoulder instability affected 21 patients preoperatively and persisted in 5 of these patients after surgery, even in the 5 patients with persistent instability who experienced some relief from the winging itself. CONCLUSION: Surgical decompression and neurolysis of the long thoracic nerve significantly improve scapular winging in appropriate patients, for whom these techniques should be considered a primary modality of functional restoration.

|
Rapid recovery of serratus anterior muscle function after microneurolysis of long thoracic nerve injury. ** Free **
Authors : Nath RK, Melcher SE.
|
BACKGROUND: Injury to the long thoracic nerve is a common cause of winging scapula. When the serratus anterior muscle is unable to function, patients often lose the ability to raise their arm overhead on the affected side. METHODS: Serratus anterior function was restored through decompression, neurolysis, and tetanic electrical stimulation of the long thoracic nerve. This included partial release of constricting middle scalene fibers and microneurolysis of epineurium and perineurium of the long thoracic nerve under magnification. Abduction angle was measured on the day before and the day following surgery. RESULTS: In this retrospective study of 13 neurolysis procedures of the long thoracic nerve, abduction is improved by 10% or greater within one day of surgery. The average improvement was 59 degrees (p < 0.00005). Patients had been suffering from winging scapula for 2 months to 12 years. The improvement in abduction is maintained at last follow-up, and winging is also reduced. CONCLUSION: In a notable number of cases, decompression and neurolysis of the long thoracic nerve leads to rapid improvements in winging scapula and the associated limitations on shoulder movement. The duration of the injury and the speed of improvement lead us to conclude that axonal channel defects can potentially exist that do not lead to Wallerian degeneration and yet cause a clear decrease in function.

|
Surgical correction of the medial rotation contracture in obstetric brachial plexus palsy.
Authors : Nath RK, Lyons AB, Melcher SE, Paizi M.
|
The medial rotation contracture caused by weak external rotation secondary to obstetric brachial plexus injury leads to deformation of the bones of the shoulder. Scapular hypoplasia, elevation and rotation deformity are accompanied by progressive dislocation of the humeral head. Between February and August 2005, 44 children underwent a new surgical procedure called the ‘triangle tilt’ operation to correct this bony shoulder deformity. Surgical levelling of the distal acromioclavicular triangle combined with tightening of the posterior glenohumeral capsule (capsulorrhaphy) improved shoulder function and corrected the glenohumeral axis in these patients. The posture of the arm at rest was improved and active external rotation increased by a mean of 53° (0° to 115°) in the 40 children who were followed up for more than one year.
There was a mean improvement of 4.9 points (1.7 to 8.3) of the Mallet shoulder function score after surgical correction of the bony deformity.
|
Contact US
|