|
Long Term Outcome
|
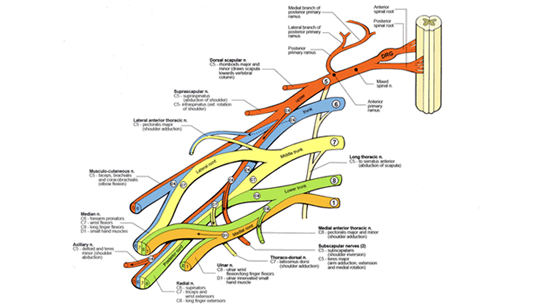
Brachial plexus injuries
cause severe functional deficits in the affected extremity.
The full extent of the arm and hand deficits may not
be known for several years.
Additionally, upper body posture may be altered
as a result of compensatory maneuvers used to deal
with poor positioning of the shoulder and arm.
|
|
"Many parents have been told that "95% of these injuries get better without treatment" . Dr. Nath's 14 years of experience, with several thousand evaluations and surgeries on children and adults with obstetric and traumatic brachial plexus injuries has led us to believe that this estimate is overly optimistic.
A recent landmark report from the Children’s
Hospital at the very well respected Karolinska Institute
in Stockholm, Sweden evaluated 105 children for functional
outcome at 5 years of age following obstetric brachial plexus
injury (Sundholm LK, Eliasson A-C, and Forssberg H. Obstetric
brachial plexus injuries: assessment protocol and functional
outcome at age 5 years.
The Swedish
study evaluated motor and sensory functions as well
as the overall use of the affected limb. The results indicated
that "the eventual outcome from in upper-plexus lesions
is more complex than is commonly believed". Occupational
Therapists and a physician specializing in movement problems
of children determined these outcomes.
The findings are quite compelling
and very much in agreement
with what we see in our clinic:
- Children
with no apparent deficits in shoulder, biceps or hand
function by 3 months of age: 70% full recovery by age
5 years.
- Children
with remaining deficits in shoulder, biceps or hand function
by 3 months of age: 5% full recovery by age 5 years.
It
is important to understand the meaning of these results:
even in the best case
scenario, where no obvious deficits remain by the age of
3 months, fully 3 out of 10 children will have significant
functional deficits by the age of 5 years if untreated.
In children with remaining problems after the age of 3 months,
over 9 out of 10 children will have residual deficits by
5 years. Overall, 66% of children, or 2 out of 3, had severe
problems by the age of 5 years.
This information
is critical in understanding the progression of the muscle
imbalances that occur following brachial plexus injury.
The 105 children in this study all received physical therapy
and primary surgery where appropriate at the age of 3 to
6 months. None of the children underwent secondary or muscle
transfer surgery by the age of 5 years.
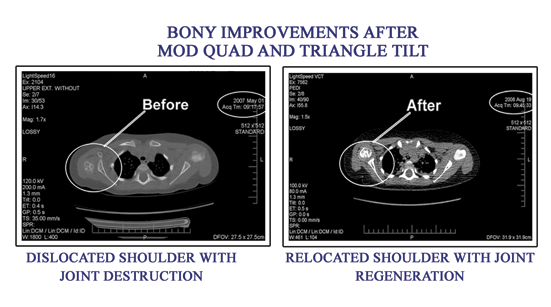
It is these residual muscle imbalances that secondary surgery (including the quad procedure) attempts to correct. The surgery moves around muscles which cause the deformity to place them in a better position for overall function. Joint deformities including dislocated shoulders are addressed in appropriate patients with the Triangle tilt surgery.
Dr. Nath has performed the Mod Quad surgery on several thousand children and adults with excellent improvement in function. Our overall improvement in arm abduction and flexion (lifting the arm over the head) has been 60-70 degrees, and in external rotation (placing the hand behind the head; throwing a ball) has been 40-50 degrees. These results have been published in several peer- reviewed scientific publications as well as Dr. Nath’s book, the only one published on management of brachial plexus injuries in children.
In summary, the arm function of children with brachial plexus injury is actually more affected than commonly thought. Even in the best group of children, those with no visible deficit by age 3 months, 30% will have residual, noticeable deficits by age 5 years. Those with visible deficits by the age of 3 months will have a 95% incidence of residual problems by age 5 years. This important study supports the idea that aggressive, including surgical, management of brachial plexus injuries may lead to better outcomes.
|